It began like this.
Early in the year, I learned that the US Air Force Museum was going to unveil the Memphis Belle B-17 exhibit in early May. I called my friend, John (of Michigan and New Orleans trips “fame”), and we began to make plans for the trip to Dayton, Ohio. Of particular interest were the three other B-17s that were going to fly in for the unveiling.
During initial planning, I realized that my manager for my ongoing writing job as editor for the Velocity News, Reiff, lives in the Dayton area. I contacted him, and explained our plans, and before I could say anymore, he promptly invited us to see his “83%” XL-RG (N142AZ). He also said we might be able to visit another builder that lived nearby.
The Velocity is a unique composite (fiberglass-plus) “home built” aircraft with more than 300 either built or under construction. Most of the owners and builders belong to their association, the Velocity Owners and Builders Association.

The Velocity is pusher/canard kit-built aircraft. (Photo: Velocity Aircraft)
Leg One of My Trifecta — B-17s
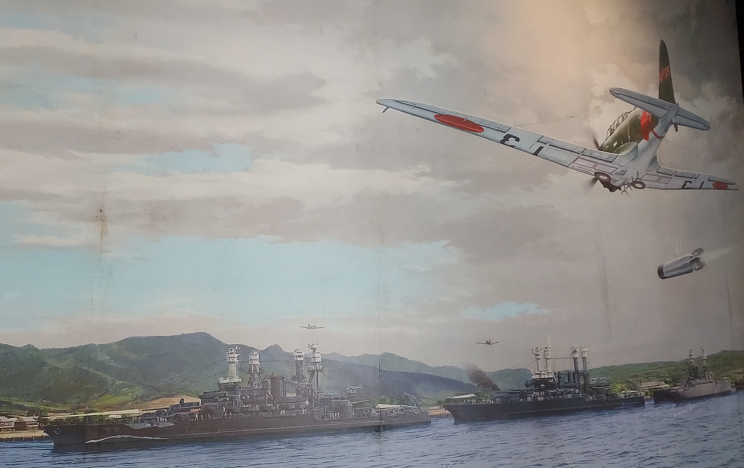
Days One and Two in Ohio were spent at the USAF Museum. John and I witnessed a formation of three B-17s and five P-51s much as it must have looked on a bombing run over Europe in 1943. They did not land because the weather outlook suggested they might not be able to take off again. On Day Two, the Memphis Belle exhibit was unveiled, the B-17s were able to come in and land, and we got to walk through two of the B-17s on the flight line.

The initial reason for our visit to the Dayton Area—the unveiling of the Memphis Belle exhibit celebrated by three of the currently 12 flying B-17s.

The Memphis Belle on Display at the USAF Museum

One of the five P-51 Mustang aircraft that participated in the B-17 fly-over.
Leg Two of the Trifecta
Early Friday morning we drove over to Reiff’s home. He greeted us and opened the garage door, revealing his “83%” Velocity XL-RG (many builders post and update their estimate of how near completion they are—Reiff feels he is “83%” to completion. “XL” indicates extra-large cabin, “RG” indicates retractable landing gear). We spent the next two hours going over the aircraft. Reiff guided us through many of the features and unique aspects of the Velocity, showing me many of the features of the aircraft we have been writing about.

Reiff greeted us in his garage.

The engine is mounted on the rear of the aircraft—a “pusher” aircraft.
Later that morning we drove to the home of Jerry and Linda who are well into the construction of their XL-RG. They were preparing to cut and fit the metal firewall in the engine compartment.
Like most tasks, before you do anything, you have to do something else first. In this case, it was to remove the right wing, move “stuff” around the shop floor, and reposition the aircraft to make room for the “cutting table.”
After lunch, the work began.
What followed looked like finely-honed teamwork: Jerry driving the nibbler (metal cutter), Linda guiding the vacuum to pick up bits of cut metal, and Reiff steadying the sheet of metal. Within a matter of minutes, the firewall was cut, and ready for fitting. The afternoon was declared a success, and we returned to Reiff’s home.

Reiff steadies the firewall material while Linda vacuums metal chips from Jerry’s metal cutter.
Of course, for pilots, at least, nothing is better (well almost) than talking about, or working on, airplanes, unless, of course you can go flying. To top off the second leg of my trifecta, Reiff drove us out to Dayton Wright Brothers Airport (KMGY) for a demonstration flight in N44VF.
There I was…

Our ride, Velocity N44VF
Unfortunately, the ceiling was only high enough to get up to pattern altitude, and the air was anything but smooth. Reiff offered me some stick time, but the bumpy conditions were such that I would not have been able to really get a good feel for the aircraft’s controls. Still, the ride was a great experience and I will be looking for another opportunity.

The iconic Velocity over-the-shoulder shot of a winglet/rudder!

Reiff and I standing in front the aircraft we had just flown.
To top off the day, Reiff had scheduled a dinner in town with five other Velocity couples, but before dinner, we had to mount the base for his ELT in the nose of his aircraft. This, like many smaller tasks, is not difficult, if you have an extra set of hands available to hold things in place.
Dinner was excellent, but most of all, I enjoyed listening to all of the experiences and plans of those who were flying or still building their Velocities. It was a great end to a great day.
A note about the Velocity: the aircraft is typically built from a kit. Anyone may build a kit aircraft, but it does have to pass an FAA compliance inspection before an airworthiness inspection will be issued so the aircraft can be flown. All home-built and kit-built aircraft must registered as ‘EXPERIMENTAL” aircraft.
Leg Three of the Trifecta
Late last year, out of the blue, as they say, I received an email from my freshman year college roommate, Chip. Over those first two semesters we had become good friends, even going to the New York’s World’s Fair, which was not far from his home in New Jersey. At school, he and I were on entirely different academic tracks, so we had no classes together. The next year I was able to obtain a room off campus, and after that, I did not see Chip often. One afternoon, I learned that he had left the college. The circumstances were not clear, and there was no explanation, but the fact is, I never heard from Chip again. Now, nearly 50 years later, I received his email. The key piece of information I learned, relative to this post, was that he too lived in Ohio, only a couple of hours away from Dayton.
As I began making plans for the trip to Dayton, I sent him a note and let him know what we were doing and that he might be close enough to meet us there. He did, and we met, again for the first time in a long time on Thursday at the Air Force Museum. We walked, talked, and looked at everything, watched the B-17s fly over again, and went out to the flight line to tour the aircraft—all the time talking about what we had been doing over the years.
Later that evening, Chip came over to our campsite to share a drink, and wide-ranging conversation that lasted well into the night. And I did learn why he left college—he was not happy with some of the most conservative—and deep seated—attitudes of the college staff, and vocally conveying his ideas to the president resulted in a mutual agreement that he might be happier somewhere else. Nearly a half century later, we are back in touch.
For a person with my interests—airplanes, friends with airplanes, and just plane (Freudian typo) long-lost friends—to score big in all areas on one short-notice trip was truly a trifecta event for me.